Patellofemoral syndrome: a new approach thanks to neuroscience
What contribution can neuroscience make to the management of patellofemoral syndrome?
I. Patellofemoral syndrome: definition
Patellofemoral syndrome accounts for 25% to 40% of sports-related knee injuries, making it a major issue in the management of knees in rehabilitation (1).
The definition of this syndrome is anterior pain at the patella. Peri-articular and peri-patellar lesions are excluded here. It is essentially a question of a bad path or "tracking" of the patella in its trochlea. We are therefore faced here with a problem of stabilisation.
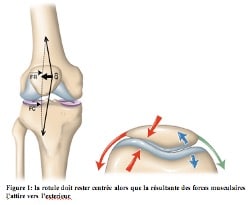
The stabilisation of the patella is essential due to the resultant of the tensile forces which have an external subluxating component (diagram).
In flexion, in addition to the better joint concordance between the patellofemoral joint, two stabilizing mechanisms are involved:
- the plating force of the patella (diagram)
- flexion alignment of the extensor system by automatic internal rotation which shifts the anterior tibial tuberosity medially.

In extension or between 0 and 15° of flexion, the constant external subluxating force is opposed by four mechanisms:
- the vastus medialis
- the outer edge of the trochlea
- the medial patellar fin
- automatic internal rotation
Anatomical abnormalities that promote poor tracking of the patella can be deduced:
- misalignment of the extensor system, in particular too external positioning of the TTA (bayonet)
- the high patella, positioned above the trochlea
- dysplasia of the trochlea (especially on the outer edge)
The stability of the patella is ensured by several elements:
- passive elements: capsule, trochlea, retinaculae, patellofemoral ligament.
- active elements: quadricipital and patellar tendon, quadriceps (especially VMO), iliotibial band.

If there is a dysbalance between all these stabilisers, there will be poor tracking of the patella.
There are also predictive risk factors for patellar femoral syndrome that we will have to work against:
intrinsic factors :
- Anatomical anomalies: dysplasia, patella alta
- Biomechanics of the lower limb
- Soft tissue shrinkage
- Muscle dysfunctions
extrinsic factors:
- sport or activity practised
- environmental condition (slope, stairs)
- type of surface
- equipment (e.g. patellofemoral stress increases with heels and decreases with barefoot running or minimalist shoes (2))
II. What kind of care?
The aim of the treatment will be to reduce the pain and improve the poor patellar tracking.
To do this, we will seek to :
- Reduce excessive stresses on the perirotal soft tissue.
- Improve strength and activation of the quadriceps (VMO).
- Correct muscle deficits in the hip and trunk.
Neuromuscular reprogramming with the Allyane method, born of neuroscience, will then have its place in this treatment.
Indeed, it will allow the treatment of the motor inhibitions found in these patellofemoral syndromes, such as the vastus medialis, which allows the stabilisation of the patella, but also the gluteus medius, which, when deficient, will lead to a dynamic valgus increasing the patellofemoral stress.
Allyane neuromotor reprogramming is a neurophysiological process that allows the modification, correction or acquisition of a motor automatism.
It is intended to facilitate the rehabilitation, modification or acquisition of a gesture in a quick and sustainable way.
To do this, we will work on the patient's proprioceptive sensations in order to make the brain aware of the deficits so as to facilitate the implementation of correction mechanisms
Then we will use mental imagery to integrate them.

1 Witvrouw E, Callaghan MJ, Stefan JJ, et al. Pa- tellofemoral pain: Consensus statement from the 3rd International patellofemoral pain research retreat held in Vancouver, September 2013. Br J Sports Med 2014; 48:411-4.
2 Bonacci J, Vicenzino B, Spratford W, Collins P. Take your shoes off to reduce patellofemoral joint stress during running. Br J Sports Med 2014;48:425-8
